d o t o r e
t o r e g . c o m
g . c o m
Dr. Mete ALPASLAN
Importance of the (frequently ignored) lead aVR
 Lead aVR looks to the heart from the right upper side and therefore better observes the right ventricular outflow tract
and the basal portion of the interventricular septum.
Lead aVR looks to the heart from the right upper side and therefore better observes the right ventricular outflow tract
and the basal portion of the interventricular septum.
Lead aVR and related pathologies
 Left Main Coronary Artery (LMCA) disease.
Left Main Coronary Artery (LMCA) disease.
 Arrhythmias.
Arrhythmias.
 Acute pericarditis: PR segment elevation and ST segment depression may be observed in lead aVR.
Acute pericarditis: PR segment elevation and ST segment depression may be observed in lead aVR.
 Dextrocardia: P wave and QRS complex will be positive (upright)
in lead aVR. Also, the normal R wave progression in anterior leads will not be observed.
Dextrocardia: P wave and QRS complex will be positive (upright)
in lead aVR. Also, the normal R wave progression in anterior leads will not be observed.
 Tension pneumothorax: PR segment depression in lead aVR and PR segment elevation in inferior leads may be observed.
Tension pneumothorax: PR segment depression in lead aVR and PR segment elevation in inferior leads may be observed.
 Acute pulmonary embolism: Lead aVR may show ST segment elevation.
Acute pulmonary embolism: Lead aVR may show ST segment elevation.
 Takotsubo cardiomyopathy: Transient ST segment elevation in lead aVR may accompany the ST segment elevation in inferior and anterior leads.
Takotsubo cardiomyopathy: Transient ST segment elevation in lead aVR may accompany the ST segment elevation in inferior and anterior leads.
Lead aVR and left main coronary artery (LMCA) disease
 If ST segment elevation in lead aVR is greater than ST segment elevation in lead V1, it may suggest LMCA disease (sensitivity 81%, specificity 80%).
If ST segment elevation in lead aVR is greater than ST segment elevation in lead V1, it may suggest LMCA disease (sensitivity 81%, specificity 80%).
 In a patient with non-ST segment elevation myocardial infarction, observation of at least 0.5 mm ST segment elevation in lead aVR suggests either
LMCA or 3-vessel disease (sensitivity 78%, specificity 86%).
In a patient with non-ST segment elevation myocardial infarction, observation of at least 0.5 mm ST segment elevation in lead aVR suggests either
LMCA or 3-vessel disease (sensitivity 78%, specificity 86%).
 Observation of ST segment elevation in lead aVR during exercise test suggests the presence of LMCA disease (sensitivity 92%, specificity 46%).
Observation of ST segment elevation in lead aVR during exercise test suggests the presence of LMCA disease (sensitivity 92%, specificity 46%).
Lead aVR and arrhythmias
 Observation of positive (upright) P waves in lead aVR during tachycardia suggests atrioventricular nodal reentry tachycardia (AVNRT).
Observation of positive (upright) P waves in lead aVR during tachycardia suggests atrioventricular nodal reentry tachycardia (AVNRT).
 Observation of a negative P wave in lead aVR suggests focal right atrial tachycardia.
Observation of a negative P wave in lead aVR suggests focal right atrial tachycardia.
 During narrow QRS complex tachycardia, observation of ST segment elevation in lead aVR suggests atrioventricular reentry due to accessory pathway.
During narrow QRS complex tachycardia, observation of ST segment elevation in lead aVR suggests atrioventricular reentry due to accessory pathway.
 In patients with Brugada syndrome, prominent R wave in lead aVR (aVR sign) may suggest increased risk of arrhythmias.
In patients with Brugada syndrome, prominent R wave in lead aVR (aVR sign) may suggest increased risk of arrhythmias.
References
 Exp Clin Cardiol 2010;15(2):e36-e44.
Exp Clin Cardiol 2010;15(2):e36-e44.
 J Am Coll Cardiol 2001;38:1355-1356.
J Am Coll Cardiol 2001;38:1355-1356.
 Int J Cardiol 2007;119:258-260.
Int J Cardiol 2007;119:258-260.
 Pacing Clin Electrophysiol 1998;21:2431-2439.
Pacing Clin Electrophysiol 1998;21:2431-2439.
 Heart Rhythm 2008;5:89-98.
Heart Rhythm 2008;5:89-98.
 Heart Rhythm 2007;4:1009-1012.
Heart Rhythm 2007;4:1009-1012.
 Ann Emerg Med 1995;26:195-201.
Ann Emerg Med 1995;26:195-201.
 Chest 1999;115:1742-1744.
Chest 1999;115:1742-1744.
 Int J Cardiol 2009;134:e97-e100.
Int J Cardiol 2009;134:e97-e100.
 Int J Cardiol 2007;119:258-260.
Int J Cardiol 2007;119:258-260.
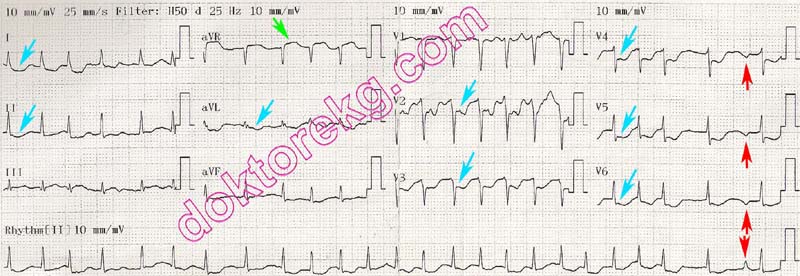
ECG 1a. The ECG above belongs to a 55 years-old woman. She was hospitalized with the diagnosis of acute myocardial
infarction and acute pulmonary edema. The ECG was recorded one hour before coronary angiography. Lead aVR shows
ST segment elevation , while most other leads show ST segment depression .
Click here for a more detailed ECG

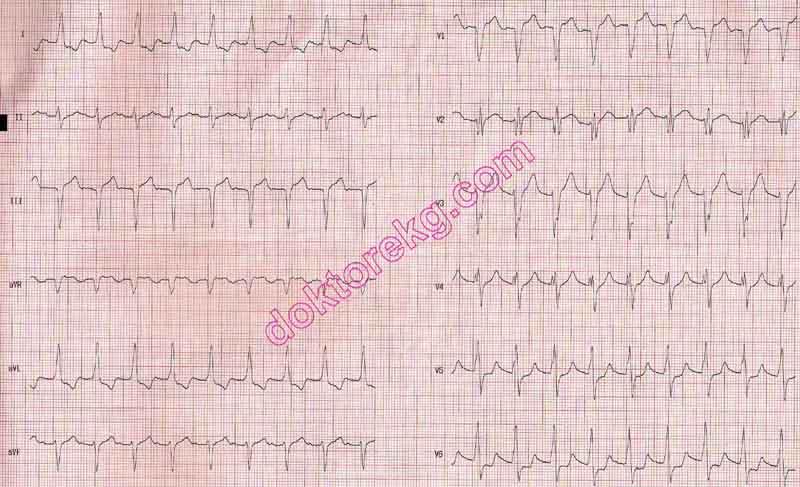
ECG 1b. Her ECG 15 minutes before coronary angiography is seen above. Albeit decreased, the ST elevation in lead aVR
and the ST segment depression in other leads persist. Medical therapy during the transfer to coronary angiography laboratory
alleviated the ECG findings. Her coronary angiography showed significant (>70%) stenosis in the LAD ostium and very
proksimal parts of the Cx and RCA.
Click here for a more detailed ECG
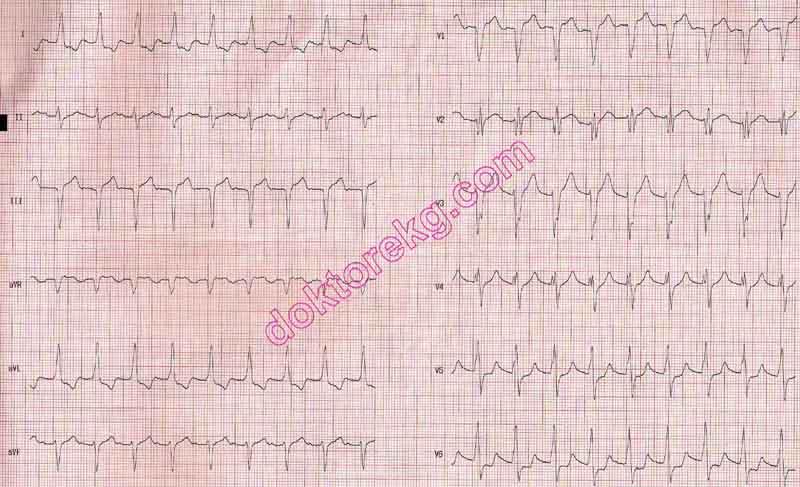
ECG 2. The ECG above belongs to a 56 years-old man who was hospitalized for acute myocardial infarction and acute
pulmonary edema. It was recorded 1 hour before the coronary angiography.
Click here for a more detailed ECG

Figure 2a. His emergent coronary angiography (left oblique caudal - spider view)
showed a short running LMCA and an LAD artery occluded at the beginning .
The Cx artery after giving the well-developed obtus marginale branch is also
completely occluded .
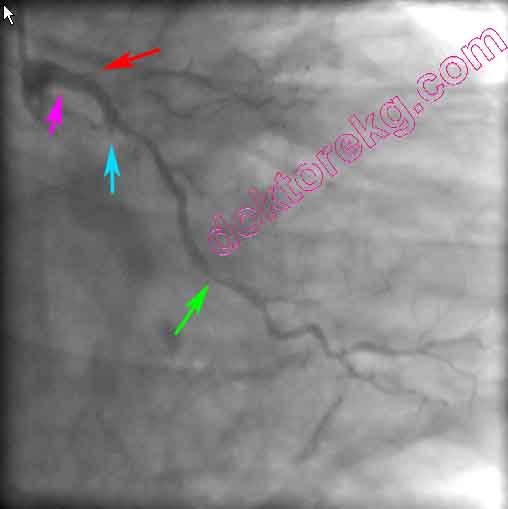
Figure 2b. The right oblique caudal view is depicted above. The LMCA is short.
LAD is occluded at the ostium . Cx is completely occluded immediately after giving
the obtus marginale branch which also has significant stenosis in the middle .

Figure 2c. The right oblique view of his right coronary artery (RCA) is seen above.
From the ostium, RCA courses only a short segment . After giving the right
ventricular branch , RCA now becomes completely occluded .

Figure 2d. After balloon angioplasty to RCA, the previously occluded segment
became visible.
ECG 3. The above ECG is from a 63 years-old man with typical retrosternal chest pain and Troponin I elevation.
Lead aVR shows ST elevation. However, no ST elevation is seen in lead V1. Most other leads show ST depression.
This presentation suggests left main coronary artery disease.
He underwent coronary angiography 15 minutes after recording of the above ECG. Left main equivalent disease was detected:
The Circumflex (Cx) artery was totally occluded after origination. There was also a 70% stenosis in the proximal LAD.
Although his left main coronary artery was normal, his lesions were left main equivalent.
Click here for a more detailed ECG

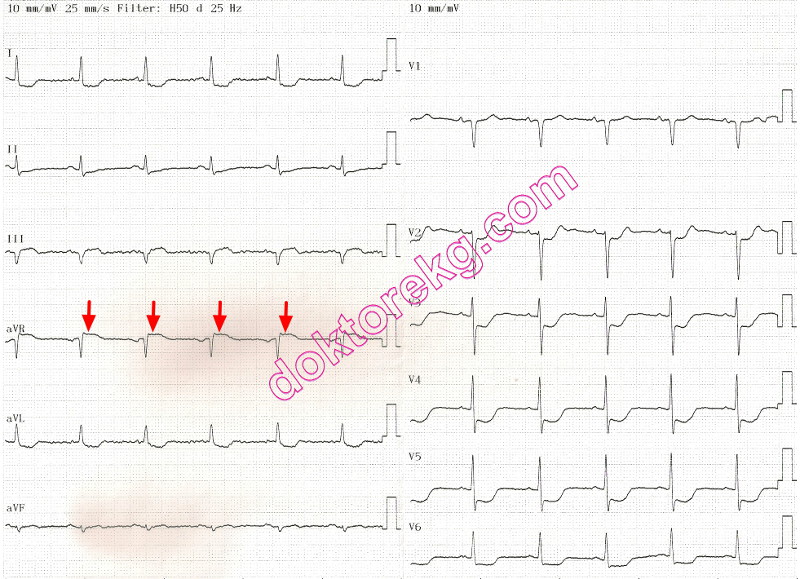
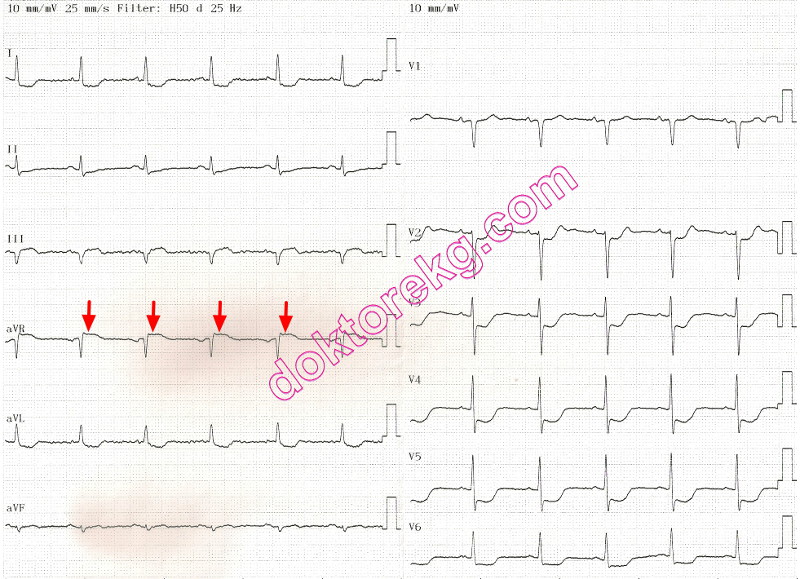
ECG 4. The above ECG is from a 78 years-old man with chest pain and Troponin I elevation.
His Troponin I level was measured as 2.2 ng/mL.
Lead aVR shows ST segment elevation while most other leads show ST depression.
Coronary angiography showed significant stenosis of the left main coronary artery.
His Circumflex (Cx) and Left Anterior Descending (LAD) arteries also had significant stenoses.
This ECG was recorded before coronary artery bypass graft surgery.
Click here for a more detailed ECG
 Lead aVR looks to the heart from the right upper side and therefore better observes the right ventricular outflow tract
and the basal portion of the interventricular septum.
Lead aVR looks to the heart from the right upper side and therefore better observes the right ventricular outflow tract
and the basal portion of the interventricular septum.
Lead aVR and related pathologies
 Left Main Coronary Artery (LMCA) disease.
Left Main Coronary Artery (LMCA) disease.
 Arrhythmias.
Arrhythmias.
 Acute pericarditis: PR segment elevation and ST segment depression may be observed in lead aVR.
Acute pericarditis: PR segment elevation and ST segment depression may be observed in lead aVR.
 Dextrocardia: P wave and QRS complex will be positive (upright)
in lead aVR. Also, the normal R wave progression in anterior leads will not be observed.
Dextrocardia: P wave and QRS complex will be positive (upright)
in lead aVR. Also, the normal R wave progression in anterior leads will not be observed.
 Tension pneumothorax: PR segment depression in lead aVR and PR segment elevation in inferior leads may be observed.
Tension pneumothorax: PR segment depression in lead aVR and PR segment elevation in inferior leads may be observed.
 Acute pulmonary embolism: Lead aVR may show ST segment elevation.
Acute pulmonary embolism: Lead aVR may show ST segment elevation.
 Takotsubo cardiomyopathy: Transient ST segment elevation in lead aVR may accompany the ST segment elevation in inferior and anterior leads.
Takotsubo cardiomyopathy: Transient ST segment elevation in lead aVR may accompany the ST segment elevation in inferior and anterior leads.
Lead aVR and left main coronary artery (LMCA) disease
 If ST segment elevation in lead aVR is greater than ST segment elevation in lead V1, it may suggest LMCA disease (sensitivity 81%, specificity 80%).
If ST segment elevation in lead aVR is greater than ST segment elevation in lead V1, it may suggest LMCA disease (sensitivity 81%, specificity 80%).
 In a patient with non-ST segment elevation myocardial infarction, observation of at least 0.5 mm ST segment elevation in lead aVR suggests either
LMCA or 3-vessel disease (sensitivity 78%, specificity 86%).
In a patient with non-ST segment elevation myocardial infarction, observation of at least 0.5 mm ST segment elevation in lead aVR suggests either
LMCA or 3-vessel disease (sensitivity 78%, specificity 86%).
 Observation of ST segment elevation in lead aVR during exercise test suggests the presence of LMCA disease (sensitivity 92%, specificity 46%).
Observation of ST segment elevation in lead aVR during exercise test suggests the presence of LMCA disease (sensitivity 92%, specificity 46%).
Lead aVR and arrhythmias
 Observation of positive (upright) P waves in lead aVR during tachycardia suggests atrioventricular nodal reentry tachycardia (AVNRT).
Observation of positive (upright) P waves in lead aVR during tachycardia suggests atrioventricular nodal reentry tachycardia (AVNRT).
 Observation of a negative P wave in lead aVR suggests focal right atrial tachycardia.
Observation of a negative P wave in lead aVR suggests focal right atrial tachycardia.
 During narrow QRS complex tachycardia, observation of ST segment elevation in lead aVR suggests atrioventricular reentry due to accessory pathway.
During narrow QRS complex tachycardia, observation of ST segment elevation in lead aVR suggests atrioventricular reentry due to accessory pathway.
 In patients with Brugada syndrome, prominent R wave in lead aVR (aVR sign) may suggest increased risk of arrhythmias.
In patients with Brugada syndrome, prominent R wave in lead aVR (aVR sign) may suggest increased risk of arrhythmias.
References
 Exp Clin Cardiol 2010;15(2):e36-e44.
Exp Clin Cardiol 2010;15(2):e36-e44.
 J Am Coll Cardiol 2001;38:1355-1356.
J Am Coll Cardiol 2001;38:1355-1356.
 Int J Cardiol 2007;119:258-260.
Int J Cardiol 2007;119:258-260.
 Pacing Clin Electrophysiol 1998;21:2431-2439.
Pacing Clin Electrophysiol 1998;21:2431-2439.
 Heart Rhythm 2008;5:89-98.
Heart Rhythm 2008;5:89-98.
 Heart Rhythm 2007;4:1009-1012.
Heart Rhythm 2007;4:1009-1012.
 Ann Emerg Med 1995;26:195-201.
Ann Emerg Med 1995;26:195-201.
 Chest 1999;115:1742-1744.
Chest 1999;115:1742-1744.
 Int J Cardiol 2009;134:e97-e100.
Int J Cardiol 2009;134:e97-e100.
 Int J Cardiol 2007;119:258-260.
Int J Cardiol 2007;119:258-260.
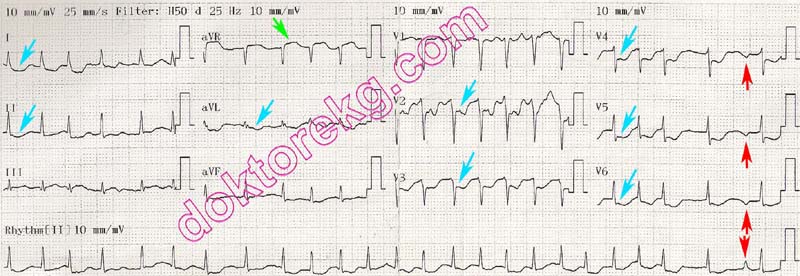
ECG 1a. The ECG above belongs to a 55 years-old woman. She was hospitalized with the diagnosis of acute myocardial
infarction and acute pulmonary edema. The ECG was recorded one hour before coronary angiography. Lead aVR shows
ST segment elevation , while most other leads show ST segment depression .
Click here for a more detailed ECG

ECG 1b. Her ECG 15 minutes before coronary angiography is seen above. Albeit decreased, the ST elevation in lead aVR
and the ST segment depression in other leads persist. Medical therapy during the transfer to coronary angiography laboratory
alleviated the ECG findings. Her coronary angiography showed significant (>70%) stenosis in the LAD ostium and very
proksimal parts of the Cx and RCA.
Click here for a more detailed ECG
ECG 2. The ECG above belongs to a 56 years-old man who was hospitalized for acute myocardial infarction and acute
pulmonary edema. It was recorded 1 hour before the coronary angiography.
Click here for a more detailed ECG

Figure 2a. His emergent coronary angiography (left oblique caudal - spider view)
showed a short running LMCA and an LAD artery occluded at the beginning .
The Cx artery after giving the well-developed obtus marginale branch is also
completely occluded .
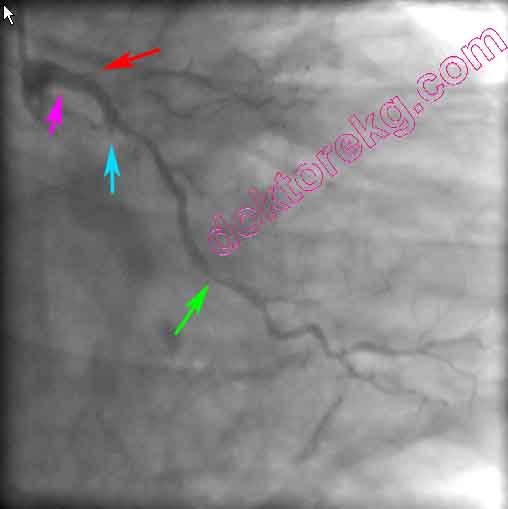
Figure 2b. The right oblique caudal view is depicted above. The LMCA is short.
LAD is occluded at the ostium . Cx is completely occluded immediately after giving
the obtus marginale branch which also has significant stenosis in the middle .

Figure 2c. The right oblique view of his right coronary artery (RCA) is seen above.
From the ostium, RCA courses only a short segment . After giving the right
ventricular branch , RCA now becomes completely occluded .

Figure 2d. After balloon angioplasty to RCA, the previously occluded segment
became visible.
ECG 3. The above ECG is from a 63 years-old man with typical retrosternal chest pain and Troponin I elevation.
Lead aVR shows ST elevation. However, no ST elevation is seen in lead V1. Most other leads show ST depression.
This presentation suggests left main coronary artery disease.
He underwent coronary angiography 15 minutes after recording of the above ECG. Left main equivalent disease was detected:
The Circumflex (Cx) artery was totally occluded after origination. There was also a 70% stenosis in the proximal LAD.
Although his left main coronary artery was normal, his lesions were left main equivalent.
Click here for a more detailed ECG

ECG 4. The above ECG is from a 78 years-old man with chest pain and Troponin I elevation.
His Troponin I level was measured as 2.2 ng/mL.
Lead aVR shows ST segment elevation while most other leads show ST depression.
Coronary angiography showed significant stenosis of the left main coronary artery.
His Circumflex (Cx) and Left Anterior Descending (LAD) arteries also had significant stenoses.
This ECG was recorded before coronary artery bypass graft surgery.
Click here for a more detailed ECG